The question of how long it takes for wood to dissolve under the skin is a complex and somewhat misleading inquiry, as wood does not naturally dissolve in biological tissue. When wood splinters or fragments become embedded in the skin, the body typically treats them as foreign objects, often encapsulating them in a protective layer of tissue or attempting to expel them through inflammation and immune responses. However, the wood itself does not break down or dissolve in the same way that biodegradable materials might. Instead, the outcome depends on factors such as the size, location, and type of wood, as well as the body's reaction. Small splinters may be naturally pushed out over time, while larger or deeper fragments may require medical intervention to prevent infection or complications. Understanding this process is crucial for proper wound care and treatment.
| Characteristics | Values |
|---|---|
| Time for Wood to Dissolve Under Skin | Wood does not dissolve under the skin. It is a foreign body and will remain unless removed surgically or pushed out by the body's immune response. |
| Body's Reaction | The body treats wood as a foreign object, causing inflammation, infection, or encapsulation (formation of a cyst or granuloma). |
| Potential Complications | Infection, abscess formation, chronic inflammation, or migration of the wood fragment. |
| Removal Methods | Surgical excision, drainage of abscess, or observation if asymptomatic and no infection. |
| Healing Time | Varies based on size, location, and infection; can take weeks to months for complete healing. |
| Prevention | Avoid embedding wood under the skin; use proper protective gear during activities involving wood. |
Explore related products
What You'll Learn

Factors Affecting Wood Dissolution
Wood embedded under the skin does not dissolve in the traditional sense; instead, the body reacts to it as a foreign object, leading to inflammation, encapsulation, or gradual degradation. The rate and extent of this process depend on several factors, each playing a critical role in how the body handles the wood. Understanding these factors is essential for predicting outcomes and managing complications.
- Wood Type and Composition: Different types of wood degrade at varying rates due to their unique cellular structures and chemical compositions. Softwoods, like pine, contain more lignin and resins, which resist breakdown, while hardwoods, such as oak, have denser fibers that slow enzymatic activity. For instance, a splinter from balsa wood may begin to show signs of degradation within months, whereas a denser wood like teak could persist for years. The presence of natural oils or tannins in certain woods can also influence the body’s inflammatory response, affecting how quickly the wood is isolated or broken down.
- Size and Depth of the Splinter: Smaller wood fragments are more likely to be fully encapsulated by fibroblasts and eventually degraded by macrophages, a process that can take 6–12 months depending on the individual’s immune response. Larger splinters, especially those deeper in the dermis or subcutaneous tissue, may remain indefinitely, as the body walls them off with collagen to prevent further irritation. For example, a 1-mm splinter near the surface might resolve within a year, whereas a 5-mm piece lodged near a joint could persist for decades without intervention.
- Individual Immune Response: The body’s ability to detect and react to foreign material varies widely. Individuals with robust immune systems may experience rapid inflammation, leading to quicker encapsulation and potential degradation of the wood. Conversely, those with compromised immunity—such as diabetics or the elderly—may exhibit delayed responses, allowing the wood to remain unaddressed for longer periods. Steroid use or autoimmune disorders can further suppress this reaction, prolonging the wood’s presence.
- Environmental and Microbial Factors: Exposure to moisture and bacteria can accelerate the breakdown of wood, particularly if the splinter introduces pathogens into the wound. For instance, a wood splinter acquired in a dirty environment might become infected, leading to abscess formation and faster degradation of the wood’s surface. However, this also increases the risk of complications like cellulitis. In contrast, a clean, dry splinter may remain stable for years without microbial intervention.
Practical Tips for Management: If a wood splinter is superficial and non-infected, monitoring for signs of rejection (redness, swelling, pus) is advisable. For deeper or larger fragments, surgical removal is often the safest option to prevent chronic inflammation. Applying warm compresses can encourage the body’s natural expulsion process, but this is only effective for small, shallow splinters. Always seek medical advice for embedded wood, especially if symptoms like fever or spreading redness occur, as these indicate infection requiring immediate attention.
Durability of Wooden Brush Rolls in Vacuum Cleaners: Lifespan Explained
You may want to see also
Explore related products

Wood Type and Skin Reaction
Wood embedded under the skin triggers a complex interplay between material properties and biological response, with dissolution timeframes varying widely based on wood type. Hardwoods like oak or maple, dense and rich in lignin, resist enzymatic breakdown, often remaining intact for years unless surgically removed. In contrast, softwoods such as pine or cedar, with lower lignin content and higher resinous compounds, may begin to degrade within months due to increased susceptibility to phagocytic activity and enzymatic digestion. This distinction highlights the importance of identifying the wood type in clinical settings, as it directly influences both the body’s reaction and the necessity for intervention.
The body’s response to foreign wood material is twofold: an initial inflammatory phase followed by encapsulation and potential degradation. Softwoods, with their higher hemicellulose content, often elicit a milder inflammatory response compared to hardwoods, which can provoke prolonged irritation due to their denser structure. For instance, a splinter of balsa wood might be encapsulated and partially degraded within 6–12 months, while a walnut splinter could remain a chronic irritant for years. Understanding these reactions is critical for healthcare providers, as it informs decisions on whether to remove the wood immediately or monitor for natural resolution.
Practical considerations for managing wood splinters under the skin depend heavily on wood type and depth of penetration. Superficial softwood splinters in non-critical areas (e.g., forearm) may be left to resolve if asymptomatic, with warm compresses applied to expedite migration to the surface. However, hardwood splinters or those embedded deeply (e.g., near joints) should be promptly removed to prevent chronic inflammation or infection. For children under 12, whose skin is more sensitive and prone to scarring, immediate removal is generally recommended regardless of wood type.
Comparatively, the role of wood moisture content and treatment cannot be overlooked. Untreated, dry wood splinters tend to remain inert, while green wood or treated lumber (e.g., pressure-treated pine) may introduce additional irritants or toxins, complicating the body’s reaction. For example, a splinter from treated decking material could cause a more severe inflammatory response than untreated cedar. Patients should be advised to disclose the source of the wood to healthcare providers, as this information is pivotal in assessing risk and treatment urgency.
In conclusion, the dissolution of wood under the skin is not a one-size-fits-all scenario but a nuanced process influenced by wood type, depth, and individual immune response. While softwoods may resolve within months, hardwoods often require intervention. Clinicians and patients alike must consider these factors to balance the risks of removal against the potential for natural resolution, ensuring optimal outcomes with minimal complications.
Durability of Wood Furniture: Lifespan, Care, and Longevity Tips
You may want to see also
Explore related products

Symptoms of Embedded Wood
Wood embedded under the skin is a foreign body that triggers a series of biological responses. Initially, the area may exhibit redness, swelling, and tenderness as the body recognizes the wood as an intruder. These symptoms often appear within hours of the wood becoming lodged. The immune system mobilizes white blood cells to isolate and neutralize the foreign material, leading to inflammation. If the wood is small and superficial, the body may encapsulate it, forming a granuloma—a protective barrier to prevent further irritation. However, larger or deeper fragments can cause prolonged discomfort and may require intervention.
Pain is a hallmark symptom of embedded wood, often described as sharp or throbbing, especially when pressure is applied. Over time, the pain may evolve into a persistent ache as the body struggles to expel or dissolve the wood. In some cases, the wood’s presence can disrupt nerve endings, causing localized numbness or tingling. If the wood is near a joint, restricted mobility or stiffness may develop, hindering daily activities. Monitoring these symptoms is crucial, as they can indicate the body’s inability to manage the foreign object on its own.
Infection is a significant risk with embedded wood, particularly if the skin was broken during the injury. Signs of infection include increased warmth, pus discharge, and fever. Wood is not sterile and can introduce bacteria or fungi into the wound, complicating the healing process. For instance, splinters from outdoor wood may carry soil-borne pathogens like *Clostridium tetani*, increasing the risk of tetanus. Prompt removal of the wood and antibiotic treatment, if necessary, are essential to prevent systemic infection, especially in immunocompromised individuals or those with diabetes.
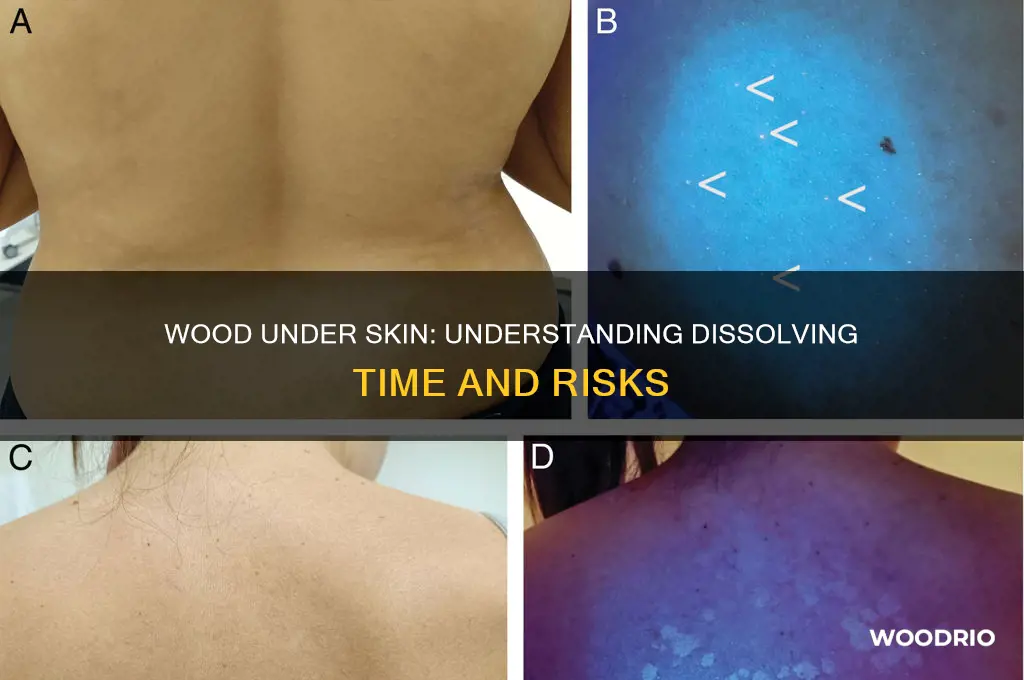
The body’s ability to dissolve wood depends on its size, type, and depth. Softwoods, like pine, may begin to break down within weeks due to enzymatic activity, but hardwoods, such as oak, can persist for months or even years. Over time, the wood may darken and become more visible beneath the skin, a process called tattooing. While some small fragments may eventually be expelled or absorbed, larger pieces often require surgical extraction. Practical tips include keeping the area clean, applying warm compresses to encourage drainage, and seeking medical attention if symptoms worsen or persist beyond 48 hours.
Wood Tick Season Duration: Understanding Its Length and Timing
You may want to see also
Explore related products
$14.66 $24.99

Removal and Treatment Options
Wood embedded under the skin presents a unique challenge due to its organic nature and potential for splintering. Unlike metal or glass, wood is biodegradable, but its dissolution rate varies widely based on factors like wood type, size, depth, and the body’s immune response. While small splinters may disintegrate within weeks, larger fragments can persist for months or even years, often encapsulated in fibrous tissue. This variability underscores the importance of proactive removal and treatment to prevent complications like infection, inflammation, or granuloma formation.
Immediate Removal Techniques
For superficial splinters, prompt extraction is the most effective approach. Sterilize the area with 70% isopropyl alcohol or iodine solution, then use a sterile needle or tweezers to grasp the splinter firmly and pull it out in the direction of entry. Avoid digging into the skin, as this can cause further damage. For deeper or fragmented wood, a healthcare professional may use a scalpel under local anesthesia to excise the material. Post-removal, apply an antibiotic ointment (e.g., bacitracin or neomycin) and cover with a sterile bandage to reduce infection risk.
Conservative Management for Retained Wood
In cases where removal is impractical or risky, conservative management focuses on minimizing complications. Topical treatments like warm compresses can encourage the body’s natural expulsion process by promoting inflammation and drawing the splinter closer to the surface. Over-the-counter anti-inflammatory medications (e.g., ibuprofen 200–400 mg every 6 hours) can reduce swelling and discomfort. However, monitor the site for signs of infection, such as redness, pus, or fever, which may necessitate antibiotic therapy (e.g., oral amoxicillin 500 mg three times daily for adults).
Advanced Interventions for Chronic Cases
Persistent wood fragments may require advanced interventions. Ultrasound or X-ray imaging can localize deep splinters, guiding surgical removal under sterile conditions. For asymptomatic, encapsulated wood, observation may be sufficient, as the body often walls off the foreign material without issue. In rare cases, laser therapy or cryotherapy can be used to break down the wood, though these methods are experimental and not widely available. Consultation with a dermatologist or surgeon is critical for tailored management.
Preventive Measures and Practical Tips
Prevention remains the best strategy. When working with wood, wear puncture-resistant gloves and long sleeves, and ensure tools are sharp to minimize splintering. For children and older adults, whose skin is more fragile, extra caution is advised. If a splinter occurs, avoid "home remedies" like glue or tape, which can introduce bacteria. Instead, focus on clean extraction or professional evaluation. Regularly inspect hands and feet, as these areas are most prone to wood injuries, and educate family members on safe wood handling practices.
Wood Therapy Results: Understanding the Timeframe for Effective Body Sculpting
You may want to see also
Explore related products

Prevention of Wood Splinters
Wood splinters can be a painful and persistent issue, especially when they become embedded under the skin. While the body may eventually break down and expel foreign objects, wood splinters often require proactive measures to prevent infection and discomfort. Understanding how to avoid these injuries in the first place is crucial for anyone working with wood or engaging in outdoor activities.
Analytical Approach:
The risk of wood splinters increases with the type of wood and the activity involved. Softwoods like pine are less likely to cause deep splinters compared to hardwoods such as oak or walnut, which are denser and more prone to splintering. Activities like carpentry, gardening, or handling untreated wooden objects elevate the risk. Wearing protective gear, such as gloves and long sleeves, significantly reduces exposure. For children under 12, supervision during wood-related activities is essential, as their skin is more delicate and prone to injury.
Instructive Steps:
To prevent wood splinters, follow these practical steps:
- Inspect and Prepare Wood: Before use, sand rough edges and seal untreated wood to minimize splintering.
- Use Tools Properly: Always cut or shape wood with sharp, well-maintained tools to create clean edges.
- Wear Appropriate Gear: Gloves made of thick, puncture-resistant material are a must. For high-risk tasks, consider eye protection and sturdy footwear.
- Keep Work Areas Clean: Regularly sweep or vacuum wood debris to avoid accidental contact with splinters.
Comparative Perspective:
Unlike metal splinters, which often require immediate removal due to rust and toxicity risks, wood splinters are less urgent but still demand attention. While metal splinters can cause tetanus, wood splinters may lead to bacterial infections like cellulitis if left untreated. Prevention strategies for wood, however, focus more on material handling and protective measures rather than post-injury treatments.
Descriptive Takeaway:
Imagine a workshop where every surface is smooth, every tool is sharp, and every worker is geared up—this is the ideal environment for splinter prevention. By treating wood with care, using the right equipment, and staying vigilant, you can drastically reduce the likelihood of splinters. Remember, prevention is not just about avoiding pain; it’s about maintaining safety and productivity in wood-related tasks.
Persuasive Conclusion:
Investing time in preventive measures is far less costly than dealing with the aftermath of a wood splinter. Whether you’re a professional carpenter or a weekend DIY enthusiast, adopting these practices ensures a safer, more enjoyable experience. Don’t wait for an injury to take action—start protecting yourself today.
Durability Unveiled: Lifespan of Composition Wood Siding Explained
You may want to see also
Frequently asked questions
Wood does not dissolve under the skin. It is a foreign object and will remain in place unless removed surgically or pushed out by the body’s immune response.
Yes, wood embedded in the skin can introduce bacteria or fungi, potentially leading to infection if not properly treated or removed.
Clean the area, try to remove the splinter with sterile tools, and seek medical attention if it’s deep, large, or causing pain/infection.
The body may push out small splinters as part of its immune response, but larger pieces often require manual removal.
If left untreated, wood under the skin can cause chronic inflammation, infection, or abscesses, potentially leading to complications if not addressed.
















































